Expert Insights on Treating Chronic Migraine
Source: Healthgrades
Life with chronic migraine can be painful and challenging, which is why it’s so important to connect with a headache specialist and find the right treatment for your specific needs. Dr. Hossein Ansari, a neurologist specializing in headache and migraine treatment, explains what he wants patients to know about managing their condition.
1. Q: What is the difference between a headache and migraine?
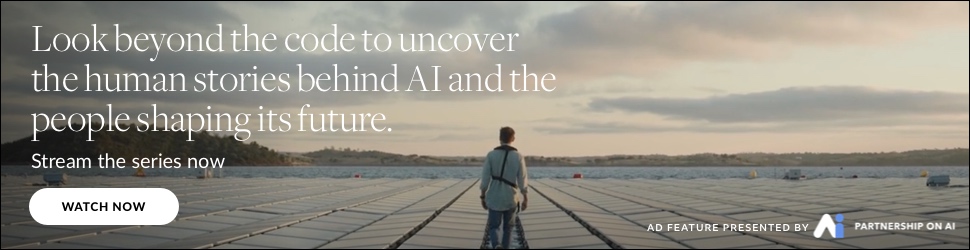
A: Migraine is a neurological disorder, and it’s not just a headache. Headache is a symptom that can occur in someone who is diagnosed with migraine. People with migraine experience moderate to severe headaches with throbbing or pulsating qualities, accompanied by nausea and vomiting, or light and noise sensitivity, or all of these symptoms together. Headache in migraine lasts more than four hours and physical activity makes it worse.
Some people experience migraine aura: visual disturbances, sensory changes, or speech problems. Aura usually comes on before headache starts.
When we diagnose someone with chronic migraine, a lot of people think that’s related to the duration of migraine–so if a patient has experienced migraine attacks for 20 years, they might think they have chronic migraine. However, we define chronic migraine by the frequency of migraine attacks per month. If a patient has 15 or more headache days each month, we classify that as chronic migraine, and treat it differently than we might treat episodic migraine, in which a patient has fewer than 15 headache days per month.
The terminology of migraine is changing; whereas once the term “migraine” was used to describe the headache and other pain associated with it, now we refer to that as a “migraine attack.” Migraine is a neurological condition, and migraine attacks are the exacerbations of this condition.
2. Q: Can migraine attacks be prevented?
A: In many cases, migraine attacks can be prevented and their frequency reduced significantly. A few years ago, we started to see some major advances in migraine prevention medications; before, we had effective options but they were all originally designed to treat other conditions. The “traditional” medications to prevent migraine include antidepressants to treat depression, antihypertensives to treat blood pressure, and anti-seizure drugs to treat epilepsy–as well as onabotulinum toxin A (Botox) injections, originally designed for cosmetic purposes. Each of these medications has been shown to prevent migraine at some level, even though they weren’t initially created to do so.
Today, we have several new medications to choose from that were designed specifically to treat migraine, called calcitonin gene-related peptide (CGRP) antagonists. They target a chemical, CGRP, that plays a role in creating the inflammation associated with migraine. By reducing CGRP levels, we can reduce the number of migraine attacks per month as well as their severity. It feels good to be able to offer patients treatments that have been designed precisely to prevent migraine attacks, and we’ve seen some excellent results with the drugs, which include erenumab (Aimovig), galcanezumab (Emgality), fremanezumab (Ajovy), and eptinezumab (Vyepti).
3. Q: How do you treat migraine attacks when they’re happening?
A: To relieve migraine pain in the moment, we have a few different classes of abortive treatments. We can prescribe ergot medications, which are delivered via infusion, nasal spray, or sublingual tablet. We also use nonsteroidal anti-inflammatory drugs (NSAIDs) like ibuprofen (Advil) and naproxen (Aleve) to help with pain. Additionally, we have triptan medications to offer, which came to the market in the 1990s and include sumatriptan (Imitrex) along with six others. They’re all available in tablet form, but some are also delivered via injection or nasal spray.
Lastly, some CGRP antagonists not only prevent migraine but can reduce symptoms in the moment as well. Ubrogepant (Ubrelvy) and rimegepant (Nurtec) are both oral tablets that can ease migraine attacks acutely, and Nurtec was actually recently approved as a preventative medication as well.
4. Q: What kind of doctor is best to treat migraine?
A: I want all people with migraine to know it’s a manageable condition when appropriately treated. It’s not curable, but it’s manageable if you have the right mindset and more importantly see the correct provider. Often, I’ll see patients who have had migraine for 20 years but their physicians kept saying, “Oh, it’s a headache, take an ibuprofen.” For many people, that’s not enough. We have so many treatment options now that no one with migraine should go without these tools. If you’re experiencing migraine attacks, it’s important to seek the care of a headache specialist. These doctors, like myself, focus their training and practice on treating people with headaches and migraine. Some are neurologists, but not all. Headache specialists can also be internists, family medicine practitioners, or even psychiatrists.
When choosing the right headache specialist, look for someone who listens to you and gives you plenty of time and attention. You want to have a full conversation with them; they need to ask a lot of questions about your experiences so they can get a good sense of what treatment plan will be best for you.